Abstract
Treatment adherence is a key factor to achieve stable glucose level in type 2 diabetes. Treatment adherence is defined as changes in lifestyle associated with self-care behaviors, like diet and exercise. The purpose of the study was to identify potentially modifiable factors based on patient illness perception associated with treatment adherence among people with type 2 diabetes and to develop intervention based on the result to increase the adherence. 152 respondents (males 37,5%, females 62,5%) were recruited from several public health institutions in Jakarta. The mean age of the study group was 57,9 years, and the mean duration of diabetes was 6,9 years. Measurements used were Self-Care Inventory Revised (SCI-R), Brief Illness Perception Questionnaire (B-IPQ), Self-Efficacy for Diabetes, and Social Support Questionnaire 6 (SSQ-6). Significant predictors of treatment adherence were self-efficacy, subscale treatment control and concern of illness perception. Based on that result, we developed 4 -session group therapy focusing on illness perception aspect, and also developed the intervention module and booklet for respondents.
Keywords: type 2 diabetes, treatment adherence, self-care behaviors, illness perception, group therapy
Introduction
Diabetes mellitus (DM) is a chronic disease, which can last in the long term, even lifetime. In 2012, DM is considered as one of the five non-communicable diseases that causing death in Indonesia (Center for Data and Information of the Ministry of Health, 2012). Prevalence of type 2 diabetes is the highest compared to type 1 diabetes and gestational diabetes, and generally more common in individuals aged 40 years and over. The primary goal of DM therapy is to achieve stable blood sugar levels (Gonzales, Esbitt, Schneider, Osborne, and Kupperman, in Pagoto, 2011). Insulin resistance experienced by patients with type 2 diabetes make the goal more difficult to achieve, because the body does not use insulin properly and difficult to keep the blood glucose at normal levels. Therefore, basically the lifestyle changes, for example related to diet and physical exercise, is an important factor in the treatment of patients with type 2 diabetes (Gonzales, et al., in Pagoto, 2011). In line with the duration of DM, adjustment and adaptation to these self-care behaviors needs to be done for a long term, even a lifetime. Stable and continuous self-care behavior is regarded as an effective therapy for type 2 diabetes disease (Mann, Ponieman, Leventhal, Halm, 2009; American Diabetes Association, 2013; Garcia-Perez, Alvarez, Dilla, Gil-Guillem, and Orozco- Beltran, 2013).
Changes in lifestyle related to self-care behaviors reflect the level of treatment adherence in type 2 diabetes. Previous study showed that level of treatment adherence on type 2 diabetes patients was still low, only in the range of 50% in developing countries (World Health Organization, 2013). Data in Indonesia also showed similar phenomenon (Ramadona 2011; Hidayat, 2013). This is primarily related to the duration of the chronic diseases that are usually very long, making it difficult to achieve stable lifestyle changes. Majority patient’s age in 40 years and over also make lifestyle changes more difficult, because in the period of middle age, people usually already formed habits such as diet, exercise, as well as settling old routine. Therefore, develop new lifestyle won’t be that easy. Gonzales, et. Al (in Pagoto, 2011) also added that adjustments to the treatment of type 2 diabetes is considered to give the burden of time and energy to the patient.
The primary aim of this study is to develop intervention to improve treatment adherence in type 2 diabetes patient. We realizes some of the earlier intervention developments for diabetes treatment weren’t emphasized on research yet to explain the process that occurs in treatment adherence (Kousoulis, Patelarou, Shea, Foss, Knutsen, Todorova, Roukova, Portillo, Pumar-Mendez, Mujika, Rogers, Vassilev, Serrano-Gil, and Lionis, 2014). Then, the first purpose of this study is to find the factors that affect treatment adherence in patients with type 2 diabetes. These factors are expected to be basis for the intervention development. The second purpose of the study is to develop intervention based to factors associated with treatment adherence in type 2 diabetes patient.
Preleminary study conducted by Wulandari and Halim (2015) with total 82 participants already found three factors associated with treatment adherence. There are subscale emotional representation from illness perception, self-efficacy and personality factors. Besides, that study also found three factor that associated by the respondents as the cause of type 2 diabetes are bad eat habits, heredity and bad lifestyle (eg. lack of sleep and lack of exercise). These study then aims as further study with the use of bigger amount of participants to make a better result. The results of further research is expected to be more precise to be the basic of intervention development. Based on preliminary study, we hypothesized that factors that associated with treatment adherence are subscale emotional representation from illness perception, self-efficacy, and one of the cognitive factors. We don’t add personality factors in this study, because on the preleminary study not all of the respondents take the personality test, because their level education was not high enough.
Theoretical Background
Researches about treatment adherence mainly focused on medication adherence, although adherence also encompasses numerous self-care behaviors that extend beyond taking prescribed medicines. Treatment adherence itself has many definitions. Some terms that used and overlapped with adherence are compliance, cooperation, concordance, and mutuality. However those terms looked patient as passive individual, so the term that eventually used is adherence. Most of the adherence definitions include elements associated with (1) the personal responsibility of patients to take care of themselves, (2) the role of the patient in the process of treatment, and (3) collaboration with health workers (Bosworth, Oddone, and Weinberger, 2006). These elements indicate that adherence means the patients play an important role and not simply obey health workers.
Definition of adherence then developed and took into account the treatment of chronic diseases, such as diabetes mellitus (WHO, 2013). Based on this, the definition of adherence to long-term therapy subsequently use the combined definition of Haynes and Rand (in WHO, 2013), the extent to which a person’s behavior – taking medication, following a diet, and/or executing lifestyle changes, corresponds with agreed recommendations from a health care provider. From this definition, we can see that treatment adherence that used encompasses numerous self-care behaviors that extend beyond taking prescribed medicines, in line with therapy that diabetes’ patients received.
Basic theory used for this study was Leventhal's Common Sense Model (CSM) (Leventhal, Brissette & Leventhal, in de Ridder and de Wit, 2006). CSM is based on the model of self-regulation, which includes the problem-solving ability and emotion regulation, both of which are directed to achieve the goals of survival and coherence (Cameron and Leventhal, 2003; de Ridder and de Wit, 2006). The strengths of this theory is the consideration of the emotional aspect, in which the other theories such as the Health Belief Model (HBM) (Rosentock, in Hayden, 2013), theory of reasoned action (Ajzen and Fishbein, in Cameron and Leventhal, 2003), and the theory of planned behavior (Ajzen, in Cameron and Leventhal, 2003) hasn’t include the emotional processes yet as an important part in understanding the self-care behavior.
Self-regulation model can be used to understand the behavior of treatment adherence, where adherence is looked as a dynamic process and have an emotional element in it. The concept of self-regulation also includes a long-term process through which a person try to achieve certain goals, and overcome the obstacles and challenges that exist in it (de Ridder and de Wit, 2006). This concept is considered suitable to explain adherence in type 2 diabetes, which also a long-term process and can even last a lifetime. By applying the model of self-regulation, the ultimate goal to be achieved in treatment adherence is to survive through maintaining good health.
The main aspect in Leventhal's CSM is illness representation, that defined as the views that a patient have about the disease. Leventhal's CSM framework see that illness representation makes each patient possessed varied views that reflect cognitive responses and emotional responses (emotional representation). Cognitive responses include symptoms (symptoms), cause (causes), duration (duration), consequences (consequences) of the disease, and treatment and control (cure and control) that can be taken against the disease.
Cameron and Leventhal (2003) added that the intervention on the basis of self-regulation could effectively improve the health and well-being of individuals. Based on CSM, patient beliefs about the disease and its treatment are motivating the decision about whether the patient would do a treatment or not (Leventhal, Brissette, and Leventhal, in Mann, Ponieman, Leventhal, and Halm, 2009). CSM theorists emphasize the potential of illness perception studies as predictors of health behavior in chronic diseases (Leventhal, Brissette, and Leventhal, in Kaptein, Bijsterbosch, Scharloo, Hampson, Kroon, and Kloppenburg, 2010). In line with the previous study (Wulandari and Halim, 2015), this study also added other factors which from the literature has shown contributes to treatment adherence or the concept of CSM. The factors are demographic factors (age, sex, level of education, marital status, and working statu), self-efficacy and social support (number and satisfaction of social support).
Some researches already developed intervention based on Leventhal’s CSM, namely Petrie, Cameron. Ellis, Buick, and Weinman (2002); and McAndrew, Musumeci-Szabo, Mora, Vileikyte, Burns, Halm, Leventhal, and Leventhal (2008). Petrie, et al. (2002) developed intervention for patients with Myocardial Infarction (MI). This intervention consists of 3 sessions (Petrie et al., 2002). The first session emphasized a description of the disease, common symptoms and terms in MI, by using images and concrete examples. The session also explored common misconception that is owned by the patient against MI. These sessions provided a cognitive improvement against these things. Second session explored the beliefs and schemes that patients have about the causes of MI. Here the patients were given proper education regarding the cause of MI and directed to understand the risk factors of MI, to increase patient confidence that he has control of the disease. Lastly, the third sessions, the patients were helped to create an action plan for handling the MI. In other research, McAndrew, et al. (2008) focused on the intervention for diabetes patient. Self-care behaviors were formed through consistent self-regulation and the use of objective blood sugar measuring device. The goal of the intervention is to build type 2 diabetes patient awareness to do the self-care behaviors consistently. These two works by Petrie el al. (2002) and McAndrew et al. (2008) would be foundation to develop the intervention in this research.
We also considered developing a group therapy intervention because it’s in accordance with the condition in Jakarta public health institution. In the group therapy, patients can more easily discuss the problems they face and be willing to accept suggestions from the facilitator who led the group rather than the individual intervention. Patients can imitate (modeling) fellow patients who are willing to exchange thoughts or feelings about type 2 diabetes. The intervention group also helps patients to realize that he/she is not alone in experiencing type 2 diabetes. The intervention group also easier to apply in health institutions in Jakarta, considered that each health institution usually has been formed support group for type 2 diabetes patients. Therefore this intervention can be implemented at their regular meeting.
Methods
Participants
Participants in this research were type 2 diabetes patients in several health institutions in Jakarta. Based on the literature, usually type 2 diabetes patients aged more that 40 years old.
Measurement
All measurement tools used in this study has been adapted in Bahasa Indonesia, and tested for validity and reliability. Measurement tools used are:
- Self-Care Inventory Revised (SCI-R) consists of fifteen items to measure the patient’s perceived adherence to diabetes self-care recommended treatment (La Greca, 2004). The scale of measurement used is a Likert scale, with a range of 1 (never) to 5 (always). SCI-R result is a global score, where higher score indicates that patients are perceived themselves obey the treatment well (Weinger, Butler, Welch, LaGreca, 2005). In this study, item 3, 10 and 15 are not included in the statistics calculation. Item 3 (”If type 1: check ketones when glucose level is high.”) and 15 (“If on insulin: Adjust insulin dosage based on glucose values, food, and exercise.”) reflects treatment adherence of type 1 diabetes. In item 10 (“Treat low blood glucose with just recommended amount of carbohydrate.”), some of the respondents answered that they have never had a low sugar, so it cannot be included in the calculation.
- Brief Illness Perception Questionnaire (B-IPQ) consists of nine items that measured aspects of the illness representation (Broadbent, Petrie, Main, and Weinman, 2006). Measurement scale used is Likert scale, ranging from 0 to10, which meaning is different. On items 1, 2, 5 6, and 8, higher score means patient perceived diabetes as threatening disease. While on items 3, 4, and 7, the lower scores means patients perceived diabetes as threatening disease. Total B-IPQ scores can be calculated and reflect the perceived level of threat by patient regarding his/ her illness. Meanwhile, the ninth item is a causal items, which responses can be grouped in categories such as stress, lifestyle and heredity, depending on the disease being investigated in the study (Broadbent, Petrie, Main, and Weinman, 2006). B-IPQ has been translated into Bahasa Indonesia (Sartono, Tahapary, Halim, and Kaptein, 2014) and tested for validity and reliability (Oktaviany, Sindunata and Angela, 2014). But the total score of illness perception cannot be used because the test results do not pass the test the validity of 2nd order, so only each of the aspect that can be analyzed in this study.
- Self-Efficacy for Diabetes consists of eight items to measure a patient’s confidence in conducting the diabetes treatment (Stanford Patient Education Research Centre, 2004). Likert scale was used with a range of 1 (not confident at all) to 5 (very confident). The higher scores indicate higher levels of individual confidence.
- Social Support Questionnaire (SSQ-6) consisted of six items used to measure social support (Sarason, Sarason, Shearin, and Pierce, 1987). SSQ-6 consists of two parts, which measures the numbers and satisfaction of social support. For both parts, the higher the score showed higher amount of social support or higher satisfaction of the individual.
Data Analysis
Data analysis used in this research is multiple regression to find factors that contributed to type 2 diabetes treatment adherence.
Procedures
We considered several things, namely considerable number of items, age of the most patients were over 40 years, and possible eye complications, then decided to give the test individually and read out loud one by one to each patient. Data collection is done every day since December 3, 2014, by visiting public health institutions in Jakarta. Researchers also aided by some fellow researchers to conduct individual testing. All of the health institution in this study was government-owned institutions, where a majority of respondents came from the middle to lower social status. Patient’s educational level was not too high so it made them difficult to understand the items. That made individual testing more suitable, because the testers can assist the respondents directly. We also got respondents through the snowball sampling to gain varying social status. For data analysis, we will use multiple regression technique by SPSS, to find factors that can predict treatment adherence in patients with type 2 diabetes.
Results
Research conducted on 152 respondents with type 2 diabetes in Jakarta. Amount of female respondents are 73% and male respondents are 27%, average age was 56.1 years (SD = 9.10), and mean duration of type 2 diabetes diagnosis was 5.7 years (SD = 6.5). Below is a description of respondents by sex, level of education, working status and marital status:
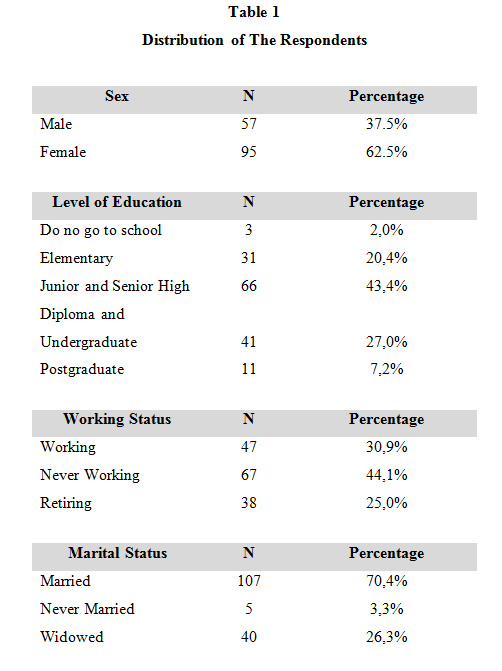
Data above showed that the majority of respondents were female (62,5%), have level of education on junior and senior high school (43,4%), never working (44.1%) and married (70,4%).
We then tried to do the interpretation of treatment adherence data by making norm reference, based on the theoretical mean and theoretical standard deviation. Based on the calculations, the category score are 0-29 (Low), 30-48 (Medium), and 49-65 (High). From these categories, it was found that 28 respondents (18,4%) are in the low adherence rate, 117 respondents (77,0%) are in the medium category, and 7 respondents (4,6%) were in the high category.
After that, we ran the correlation technique first, and find three factors that correlate significantly with treatment adherence, namely self-efficacy, treatment control and concern aspect of illness perception.
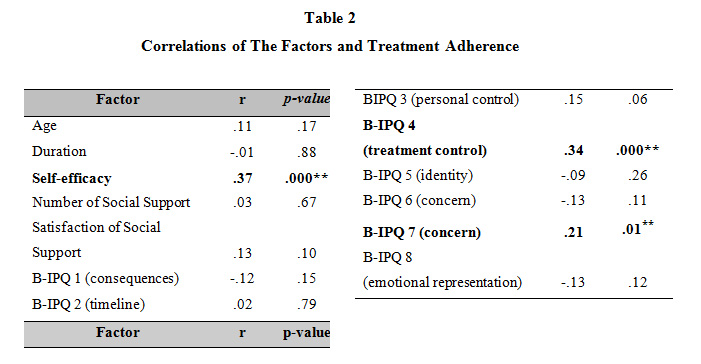
The analysis continued with multiple regression, which found that all the three factors that correlates significantly can predict treatment adherence in type 2 diabetes.
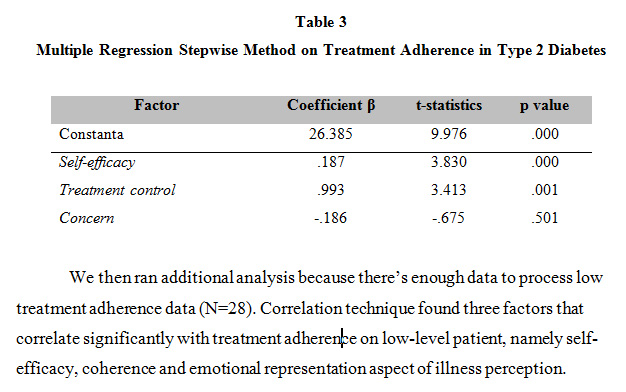
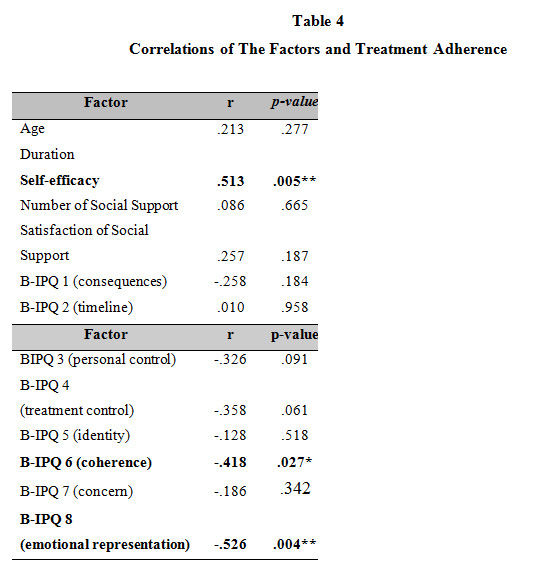
We then ran additional analysis because there’s enough data to process low treatment adherence data (N=28). Correlation technique found three factors that correlate significantly with treatment adherence on low-level patient, namely self-efficacy, coherence and emotional representation aspect of illness perception.
 ] ]
Discussion
Results showed that the respondents’ treatment adherence is relatively homogeneous in medium level (77%). Medium level treatment adherence indicates that respondents basically already know self-care behaviors that should be done, but they have not done it in accordance with the recommended frequency.
This result is quite different from the pervious researches’ findings, which suggests that long-term adherence to type 2 diabetes therapies is low (Ramadona 2011; Hidayat, 2013; WHO, 2013). Although preliminary study also found medium level of treatment adherence from the respondents. Data collection that being done in health institutions possibly making the respondents encountered were patients who already have a routine for checking their condition. This possibly caused the data homogeneous in medium level.
The level of treatment adherence also may be explained by description of illness perception among respondents. Illness perception aspects that can predict treatment adherence are (1) the more patient think the treatments are helpful (treatment control), and (2) the more they can control their worry (concern), the more they adhere to treatment. In other side, on low-level treatment adherence patient, illness perception aspects that correlate significantly are (1) the more they understand about the disease (coherence), and (2) the more they can control their negative emotion (emotional representation), the more they adhere to treatment.
Furthermore, based on a brief interview conducted on 5 respondents with high levels of adherence, the researchers found that respondents consider diabetes as a “serious” disease because of severe complications that can occur (consequences). In addition, they also have a pretty good understanding about the diabetes and procedures for treatment (coherence), and felt that the medicines help (treatment control), so they encouraged to do the self-care behaviors. Interview on high-level respondents showed that they have their own monthly personal note (not the records from health institution) regarding blood sugar levels, take medications regularly and in line the proper dosage, exercise at least three times a week, reduce the portion of food, especially rice, and replace it with brown rice, potatoes or yams, and also regular visits to the doctor at least once a month. They also have stable low blood sugar, which is below the 200 mg / dL per month.
From these results, we concluded that treatment control, coherence and consequence, and also emotional aspect of diabetes, are illness perception aspects related to diabetes treatment adherence. We found that the respondents generally quite understand about diabetes self-care behaviors and aware of its benefits, but they do not assume type 2 diabetes as a life threatening disease. This means that the patients actually understand what they had to do, but diabetes is not a serious illness for them, so they do not feel the urge to keep overly strict diet, or do not fell that they need to exercise too regularly as recommended by doctor. The implication for intervention then, the patient need to be more realize that diabetes has a great influence on their lives and can cause serious complications that need to be prevented.
From the findings, emotional aspect also plays an important role in diabetes treatment adherence. Sudden diabetes diagnosis is often considered as traumatic event, and even caused anxiety (Hauser and Pollets, 1979). Therefore, patient usually feels grief in early diagnosis stage. Next, the common stage is denial, when the patient rejects the reality of diagnosis that they have (International Diabetes Federation, 2013). At this stage the patient can assume that type 2 diabetes disease is not a serious illness, or trying to get away from the fact that he/she had diabetes (International Diabetes Federation, 2013). The last stage is acceptance, where the patient accepts his/her condition. Then, we concluded that it is important to identify emotional responses and emotional stages that are experienced by patients. After identification, the patient should be helped to gradually enter the stage of acceptance (acceptance). Furthermore, the respondents can also learn ways to manage their negative emotions, such as fear or anxiety. In line with this, a study conducted by Hidayat (2011) on diabetes patient in Bogor hospital showed that there were a relationship between emotional coping techniques and the level of treatment adherence. Respondents who have adaptive coping techniques had 2.735 times the chance for adhering the treatment compared to patients with ineffective coping techniques (Hidayat, 2011).
Illness perception is part of self-regulation process. In this research, self-regulation defined as process oriented in achieving good health (Cameron and Leventhal, 2003; de Ridder and de Wit, 2006), through problem solving, emotion regulation, and evaluation based on strategy and goals that already achieved (Maes dan Karoly, dalam Caltabiano dan Ricciardelli, 2013). These results above showed that patients with type 2 diabetes who have (1) a good understanding of diabetes and procedures for treatment, (2) thought that medicines helps, (3) realize that diabetes is a disease of "serious" disease and can cause many complications, and (4) manage their emotion, can have a good self-regulation and manage treatment adherence well.
Patients may realize that comply with the appropriate treatment, such as taking medication regularly and keep the diet every day, will help achieve the goal of good health. Then when the patient checks blood sugar level regularly, patients can obtain positive consequences, namely a stable blood sugar level. As a result, patients realize the treatment adherence that she/he was doing was right, give good results, and make patients more determined to continue obey the doctor’s recommendation. A flow of self-regulation like this, will further affect the patient's emotional aspects. Fears and worries can be decreased, because patients feel that the course of treatment he/she is doing is right, although the possibility of worries and concerns still remains because the fear of complications. At this stage, the worries and concern should be retained as long as it is keeping the patient do the treatment adherence.
Self-efficacy was found as a factor that has the strongest correlation and can predicts treatment adherence. The previous studies also found in line result (Mann, et al., 2009; Wulandari and Halim, 2015). Self-efficacy is defined as the extent to which the patient feels confident that he/she can control their diabetes through the treatment adherence. Self-efficacy of Bandura (1977) is basically considered as a concept that affects the formation of self-regulation (de Ridder and de Wit, 2006). By definition, this two concepts was nearly identical, in which self-efficacy is defined as an individual's belief to perform behaviors that can be achieved and the expectation that the results will become a reinforcement (Bandura, 1977). In relation to self-regulation, self-efficacy is considered to affect level and type of objectives that individual want to achieve, performance standards and strategy given, in this case is related to how the patient is doing diabetes self-care behaviors (Cervone, Mor, Orom , Shadel & Scott, in de Ridder and de Wit, 2006).
Individuals with higher self-efficacy are probably more confident to do the diabetes treatment. Diabetes treatment itself is a complex procedure, including monitor blood sugar levels, follow diet recommendation and physical exercise regularly, taking care of the health of the feet, attend scheduled appointment with a doctor, routine checks for the presence of complications such as eye, as well as taking oral medications or injection regularly (Anderson, in Pagoto, 2011; Schechter and Walker, 2002). Actually, its complexity can make patients reluctant and unsure to do the treatment well. Therefore, in the development of treatment adherence interventions, we need make the material as easy as possible for patient understand, to increase patient’s self-confidence and make them feel able to perform that treatments.
Intervention will be developed by exploring factors from the results and also add social support factors, although there was no significant correlation. We considered the nature of diabetes treatment adherence that should be done continuously, so family or friends can help remind the patients, such as taking medication and maintaining the diet. In addition, patients with type 2 diabetes usually will get rapid cognitive decline, especially in the memory function (Ruis, Biessels, Gorter, Donk, Kappelle, and Rutten, 2009; Downs & Faulkner, 2015), so they will need help and support from the caregivers.
We also developed intervention in the form of group therapy. In the group intervention, patients can discuss the problems they face more easily and be willing to accept perspective and suggestion from the facilitator, rather than individual intervention. Patients can imitate (modeling) fellow patients who are willing to exchange thoughts or feelings about type 2 diabetes. The intervention group also makes patients realize that he/she is not alone in experiencing diabetes.
The intervention group also easier to apply in health institutions in Jakarta, because each health institution usually has been formed support group of type 2 diabetes patients. Therefore, the intervention can be done at their regular meeting. Additionally, development of intervention also needs to consider differences in socio-economic background and educational status of the patient. So the intervention modules will also be divided based on the patient's background.
Intervention
CSM concept see that chronic disease patients have a "mental tools" used to evaluate the meaning of a sensory stimulus that he/she experienced, including evaluation related to disease’ duration, severity, location, etc. (Cameron and Leventhal, 2003). This "mental tools" is called illness perception, that turns affect the patient's emotional state and influence what will the patient do to physical symptoms he/she experienced.
This research’ results found that aspects of illness perception that can predicts treatment adherence are treatment control, coherence, consequence, and also emotional aspects. The other factor is self-efficacy. Then the intervention aims are providing a clear and complete understanding of diabetes treatment, rising patients’ awareness of the importance and benefits of doing diabetes self-care behaviors, emphasizing dangers and clinical consequences of type 2 diabetes, and helping increase patients’ confidence that they can control their own physical condition.
This intervention are based on two previous studies that developed intervention based on Leventhals’ CSM. The first study are Petrie, Cameron, Ellis, Buick, and Weinman (2002) to patients with Myocardial Infarction (MI), and the second one are interventions for patients with diabetes mellitus (DM) type 2 (McAndrew, Musumeci-Szabo, Mora, Vileikyte, Burns, Halm, Leventhal and Leventhal, 2008).
This two studies emphasized about subjective physical symptoms experienced by patients with type 2 diabetes. Patients with type 2 diabetes, as well as patients with other diseases, tend to make subjective physical symptoms they experienced as a form of identification (identity aspect) of the type 2 diabetes disease (Wagner, Schnoll, and Gipson, in McAndrew, et al., 2008). Examples of subjective physical symptoms are headache, frequent urination, and itching, where the patients only rely on it. It means that the patients only focus on their subjective physical symptoms, then they feel the need to care for themselves only when their body felt sick.
Therefore, behavioral treatment of diabetes needs to be made specifically, which covers how and when to conduct the treatment (aspects of the timeline). For example, not only set a healthy diet, but food intake must be adjusted to the type and weight of the body and right calories to make blood sugar levels stable (McAndrew, et al., 2008). Another example is the behavior of sport, which is made by determining the specific activity (such as walking), and duration of exercise.
In additions, we also added session about emotional regulation (Gratz and Roemer, 2004). This approach is different with conventional tendency to restrict the expression of emotion and disruption of the process of emotion regulation.
Gratz and Roemer (2004) developed a new approach, in which emotion regulation is not equated with a "control", but acceptance of emotion. This approach includes several dimensions, namely (1) awareness, understanding, and acceptance of emotions, (2) ability to engage in behavior that aims to limit impulsive behaviors, when faced with negative emotions, (3) ability to use the right strategies to modify the intensity or duration of the emotional response, rather than entirely eliminate emotion, and (4) willingness to experience negative emotions as part of the pursuit of meaningful activities in life (Gratz and Roemer, 2004).
First session contains implementation of pre-test for patient, followed by explanation about diabetes, particularly about type 2 diabetes. The explanation consists of common symptoms, clinical consequences, and common terms. The session also explores trust and misinformation (a common misconception) that is owned by the patient against diabetes, which can provide a cognitive improvement against it (Petrie, et al., 2002). The method for exploring a common misconception is Myths and Facts.
Second session contains of explanation about risk factors that patients assumed about type 2 diabetes. This session explores the beliefs and schemes that patients have about the causes of diabetes. Here the patient is given proper education regarding the cause of diabetes and directed to understand the risk factors for diabetes and increase patient confidence that he/she has control of the disease.
Third session explores emotional aspects of diabetes. It explains about negative emotions, and the emotion regulation techniques that patient can do. The important thing is to help the patient to identify their emotions themselves. This can help patients to understand themselves better, as well as the process of acceptance of the emotion or the diabetes conditions that he/she experienced. Patients will also be given advice regarding activities that may increase the occurrence of positive emotions. This session ends with relaxation from the facilitator, to help the patient exercise to cool down the arousal of the emotion.
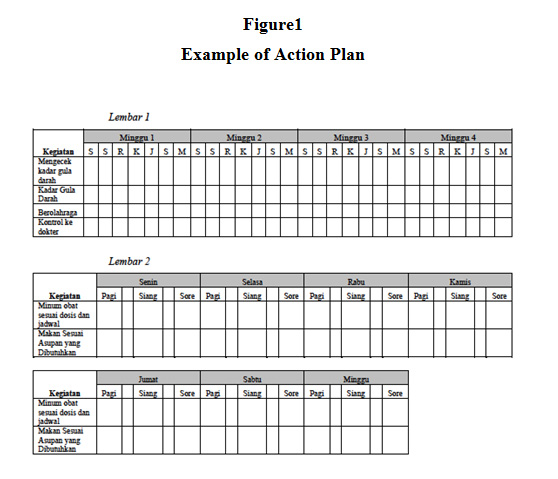
Fourth session helps patients determining their coping mechanism and making an action plan for handling their type 2 diabetes (Figure 1). For patient with low socio-economic status, we give table consists list of self-care behaviors. Then patient just need to check the box, every day, depends on the self-care behaviors. In other side, patient with high socio-economic status is not given the table, but the instruction to make their own action plan.
In addition, this session also emphasizes the use of objective measuring blood sugar tools, which can be used by patients at home. The use of this tool allows patients to see a direct relationship between the treatment behaviors that he/she did (for example regulate food intake) with the good output, namely stable blood sugar levels (causal aspect). It also worked as reinforcement for the patient (consequences). This will strengthen the self-care behavior. But this information is given only for high socio-economic status patient, due to the price of the tool.
As mentioned above, this intervention also includes session for caregivers of diabetes patients. The objectives of the session are (1) caregiver understands self-care behaviors that patient should be done at home (2) caregiver understands the emotional state and cognitive decline that may be experienced by patients with type 2 diabetes, and understands how to respond (3) caregiver understands their role as observer and reminder for the patient to do the necessary self care behavior.
This intervention is accompanied with set of module and booklet for the patient, that contains explanation and material that given in the sessions. The booklet can be brought home for the patient, to help them follow the self-care behaviors continuously.
Conclusion
Based on this study, we can conclude that illness perception aspects were correlated significantly with type 2 diabetes treatment adherence, along with self-efficacy factor. We also found that particular belief that affects treatment adherence was the patient do not assume type 2 diabetes as a life threatening disease. Then, for the intervention, it is important to raise patient’ awareness about the danger and serious complications of type 2 diabetes disease and how to manage it. The diabetes treatment procedures also have to be given very clearly and concrete for the patient.
RBibliography
American Diabetes Association. (2013). Standards of Medical Care in Diabetes. Diabetes Care, 36 (Suppl 1), 11–66.
Bandura, A. (1977). Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review, 84, 191–215.
Bosworth, H. B., Oddone, E. Z., dan Weinberger, M. (2006). Patient Treatment Adherence: Concepts, Interventions, and Measurement. New Jersey: Taylor and Fracis e-Library. Accessed September, 15th 2014 from http://books.google.co.id/books?id=goF5AgAAQBAJ&printsec=frontcover#v=onepage&q&f=false
Broadbent, E., Petrie, K. J., Main, J. & Weinman, J. (2006). The Brief Illness Perception Questionnaire. Journal of Psychosomatic Research, 60, 631–637.
Caltabiano, M. L. & Ricciardelli, L. A. (2013). Applied topic in health psychology. Oxford: John Wiley & Spns, Ltd.
Cameron, L. D. & Leventhal, H. (2003). The self-regulation of health and illness behavior. London: Routledge.
Center for Data and Information of the Ministry of Health. (2012). Buletin jendela data dan informasi kesehatan: Penyakit tidak menular. Jakarta: Indonesia Ministry of Health..
de Ridder, T. D. & de Wit, J. B. F. (2006). Self regulation in health behavior. West Sussex: John Wiley & Sons Ltd.
Downs, C. A. & Faulkner, M. S. (2015). World Journal Diabetes, 6 (4), 554-565.
Garcia-Perez, L., Alvarez, M., Dilla, T., Gil-Guillem, V., & Orozco-Beltran, D. (2013). Adherence to Therapies in Patients with Type 2 Diabetes. Diabetes Therapy, 4, 175-194.
Gratz, K. L. & Roemer, L. (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment, 26 (1), 41-54.
Hauser, S. T. & Pollets, D. (1979). Psychological aspects of Diabetes Mellitus:
A critical review. Diabetes Care, 2 (2), 227-232.
Hayden, J. A. (2013). Introduction to health behavior theory (2nd ed.). Massachuttes: Jones & Bartlett Publishers.
Hidayat, F. (2013). Hubungan koping individu dengan tingkat kepatuhan penyandang diabetes mellitus sebagai anggota Persadia cabang RSMM Bogor. Depok: Fakultas Ilmu Keperawatan Program Studi Magister Ilmu Keperawatan Universitas Indonesia.
International Diabetes Federation. (2013). IDF diabetes atlas (6th ed). Brussels: Internatioal Diabetes Federation.
Kaptein, A.A., Bijsterbosch, J., Scharloo, M., Hampson, S. E., Kroon, H. M., & Kloppenburg, M. (2010). Using the common sense model of illness perceptions to examine osteoarthritis change: a 6-year longitudinal study. Health Psychology, 29 (1), 56-64.
Kousoulis, A. A., Patelarou, E., Shea, S., Foss, C., Knutsen, I. A. R., Todorova, E., Roukova, P., Portillo, M. C., Pumar-Mendez, M. J., Mujika, A., Rogers, A., Vassilev, I., Serrano-Gil, M., dan Lionis, C. (2014). Diabetes self-management arrangements in Europe: a realist review to facilitate a project implemented in six countries. BMC Health Services Research, 14, 453-470.
La Greca, A. M. (2004). Manual for the Self Care Inventory. US: University of Miami September.
Mann, D. M. Ponieman, D., Leventhal, H. & Halm, E. A. (2009). Predictors of adherence to diabetes medications: The role of disease and medication beliefs. Journal of Behaviorla Medicine, 32, 278-284.
McAndrew, L. M., Musumeci-Szabo, T. J., Mora, P. A., Vileikyte, L., Burns, E., Halm, E. A., Leventhal, H., & Leventhal, E. A. (2008). Using the common sense model to design intervention for the prevention and management of chronic illness threats: From description to process. British Journal of Health Psychology, 13, 195-204.
Oktaviany, A., Sindunata, E. & Angela, L. (2014). Analisis Faktor Brief Illness Perception Questionnaire (B-IPQ) Bahasa Indonesia. Jakarta: UNIKA Atma Jaya.
Pagoto, S. (2011). Psychological co-morbidities of physical illness: A behavioral medicine perspective. New York: Springer Publishing.
Petrie, K. J., Cameron, L. D., Ellis, C. J., Buick, D. & Weinman, J. (2002).Changing illness perceptions after Myocardial Infarction: An early intervention randomized controlled trial. Psychosomatic Medicine, 64, :580–586.
Ramadona, A. (2011). Pengaruh konseling obat terhadap kepatuhan pasien diabetes mellitus tipe 2 di Poliklinik Khusus Rumah Sakit Umum Pusat Dr. M. Djamil Padang. Padang: Program Pascasarjana Universitas Andalas.
Ruis, C., Biessels, G. J., Gorer, K. J., Donk, Maureen, V. D., Kappele, L. J. & Rutten, G. E. H. M. (2009). Cognition in the early Stage of type 2 Diabetes. Diabetes Care, 32 (7), 1261-1265.
Sarason, I. G., Sarason, B. R., Shearin, E. N. & Pierce, G. R. (1987). A brief measure of social support: Practical and theoretical implications. Journal of Social and Personal Relationships, 4, 497-510.
Sartono, E., Tahapary, D. L. Halim, M. S. & Kaptein, A. (2014). B-IPQ Bahasa Indonesia. Accessed November 20th, 2014 from http://www.uib.no/ipq/pdf/B-IPQ-Indonesia.pdf
Schechter, C. B. & Walker, E. A. (2002). Improving adherence to diabetes self-management recommendations. Diabetes Spectrum, 15 (3), 170-175.
Stanford Patients Education Research Center. (2004). Self-Efficacy for Diabetes. Palo Alto: Stanford Patients Education Research Center.
Weinger, K., Butler, H. A., La Greca, A. M. (2005). Measuring diabetes self-care: A psychometric analysis of the Self-Care Inventory-revised with adults. Diabetes Care, 28 (6), 1346-1352.
World Health Organization. (2003). Adherence to long term therapies: Evidence for action. Geneva: World Health Organization.
Wulandari, A. & Halim, M. S. (2015). Faktor-Faktor yang mempengaruhi kepatuhan pengobatan pada pasien Diabetes Mellitus Tipe 2: Studi Pendahuluan. Jurnal Psikologi Klinis Indonesia, 1 (1), 1-11.
|
